To stent or not to stent has recently become public news with the release of the ISCHEMIA study. This study has create headlines like this one from The Washington Post:
“Stents and bypass surgery are no more effective than drugs for stable heart disease, highly anticipated trial results show”
or this headline from CBS News:
“Medication and lifestyle changes could be as effective as surgery for heart disease, trail finds”
This newly released trial was led by researchers at NYU Grossman School of Medicine and Stanford University. They looked at over 5,000 patients who had heart blockages but were stable. And what they found can be summarized as follows:
-
Placing a stent in a patient with stable blockages could improve a patient’s quality of life by reducing their symptoms like chest pain.
-
But when compared to taking medications or implementing lifestyle changes, stenting didn’t lower their risk of a heart attack or stroke.
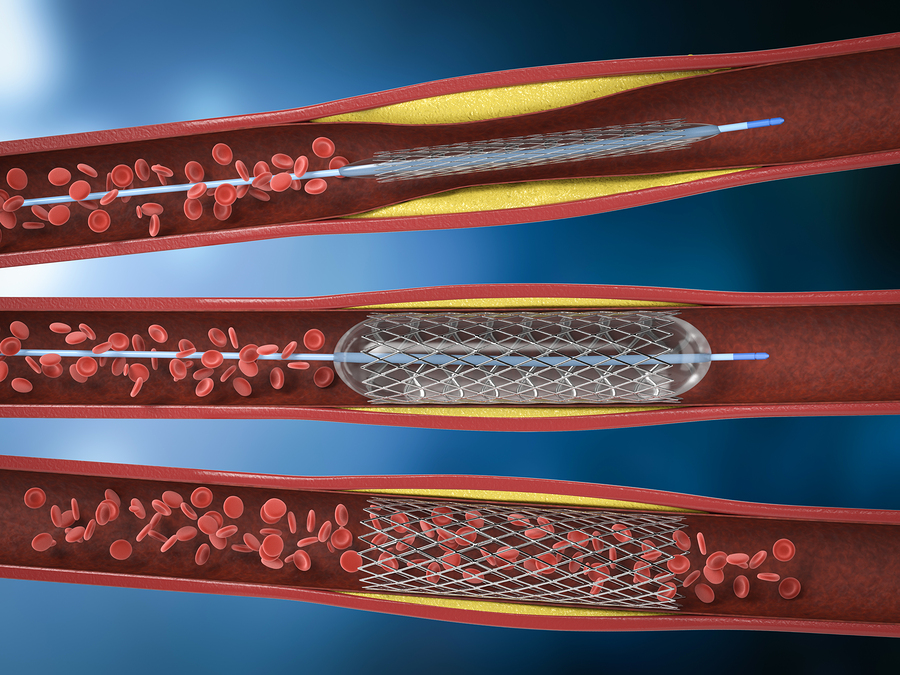
Needless to say this study has caused a significant reaction in the medical community. According to Harvard Medical School “about 600,000 people in the United States undergo an angioplasty to widen a narrowed coronary artery, nearly always with a tiny wire mesh tube (stent) left inside the artery to keep it open.”
This is not an inexpensive procedure.
To Stent or Not To Stent – The Numbers
The average cost for this procedure (angioplasty with the placement of a stent) is around $29,000.
This means that this medical procedure is a 17.4 billion dollar industry. It’s a major income stream for both interventional cardiologist and hospitals.
In response to the release of this study Elliot Antman, a cardiologist at Brigham and Women’s Hospital made the following statement:
“The ISCHEMIA trial shows that an early invasive approach does not protect patients against death or the overall chance of a heart attack, but does effectively relieve chest pain – the more chest pain a patient has, the more likely they are to benefit.”
Now before we demonize interventional cardiologist and hospitals it’s important to note the following key words that apply to this trial:
“. . .who had heart blockages but were stable.”
Stable heart blockages is the key piece of information.
Going back to the Harvard Medical School they estimate that approximately “two-thirds of these procedures are done in people experiencing a potentially life-threatening event – a heart attack or unstable angina, defined as severe, worsening chest pain during exertion or stress, or chest pain that happens at rest.”
One-third of 600,000 is 198,000 people who might find other alternatives like medications and lifestyle changes to be as effective as stenting in keeping themselves alive. That could be a 5.7 billion dollar savings per year.
To Sent or Not To Sent – What is Stable Heart Blockages
Most vascular blockages are due to a process called atherosclerosis. This usually starts with very low density lipoprotein (bad cholesterol) being oxidized by free radicals. This creates inflammation and damage to the endothelium resulting in plaque formation. Over time this plaque continues to grow, which narrows the inside of the artery.
There is usually a fibrous cap to this plaque. This fibrous cap provides structure to the plaque.
However, unstable plaque or vulnerable plaque has a thin fibrous cap usually formed from a collection of white blood cells and lipids like bad cholesterol. And if free radical damage is continuing to occur, then the resulting inflammation makes this cap even more vulnerable for a rupture.
This rupture can then form a blood clot, or release cellular debris, that can then lead to a blockage resulting in a heart attack or stroke. If you remember Tim Russert from Meet The Press, then his heart attack and death would be a good example of this process.
There are certain biomarkers that can help you and your physician determine the increased probability of plaque being unstable. They are:
c-Reactive Protein
Oxidized LDL
Both of these are due to inflammation. Oxidized LDL is usually due to free radical damage.
Which gives a strong clue to lifestyle changes that can address this. One lifestyle change would be to significantly increase your intake of fruits, vegetables, and herbal extracts that are powerful antioxidants.
As well as eliminating as many omega 6 fatty acids from your diet and replacing them with omega 3 fatty acids.
Sugar and highly processed foods also contribute to vascular inflammation.
These 3 lifestyle changes can significantly improve your health while reducing the potential for oxidized LDL and vascular inflammation. All of which can help to stabilize any plaque in the vascular system.
And as I’ve share multiple times in previous articles, nitric oxide therapy can help to vasodilate the vascular system for improved blood flow. This would then help those who are experiencing chest pain and angina.